Welcome to Blooming Littles, friends. This blog post is a little different from what we usually share around here. Typically we’re chatting about decreasing your baby’s stress, ways to help them develop coping skills, or debunking NICU myths.
Instead, I want to share a little bit of my heart and personal experience going from NICU occupational therapist to NICU mom.
As a mini introduction, my name is Katie and I’m a NICU occupational therapist, and one of the minds behind Blooming Littles.
Let’s start with a vulnerable confession.
Something can happen when you work in the NICU. You can forget it’s an intensive care unit. You can grow a little numb to the realities of parents who witness their child with invasive medical lines and tubes. You can grow disconnected from the trauma experience. I think this is a self-preservation mechanism that kicks in to help us work in an environment with such hard personal situations.
And as someone who LOVES advocating for the experiences of families, I’m also guilty of minimizing the trauma experience of the NICU.
Sometimes, our words and approach can fall closer to toxic positivity, because we don’t acknowledge the full weight of what we are witnessing or experiencing every day at work.
I promise! It’s not on purpose.
I want to start off by sharing a little bit about my birth experience.


birth story
In December 2021, I watched my son get whisked away right after birth by the same care team I had collaborated with as a NICU occupational therapist earlier that day. At 37 weeks and 4 days pregnant, I was waiting for some lab results to return. I got a call from my OB office while walking out of work on a Friday.
“Hey Katie, your labs are elevated. We have a bed for you and are going to induce you tonight.”
Ummmm, okay.
Short story, I was induced, started laboring extremely quickly, had a partial placental abruption, delivered in a half of a push, and little buddy came out eyes wide open and a shade of purple meets grey.

Thankfully, I had AMAZING infant stabilization nurses walking me through what they were doing with my new baby over on the warmer bed. They calmly and quickly communicated with me as they delivered oxygen and provided care to my newest babe. But, I knew the moment I saw my baby that he was going to the NICU.
If there’s a positive to working in the NICU and having a NICU baby, that was it.
When I saw his coloring and heard his breathing, I knew.
Minutes later, one of the neonatologists I work with regularly came and told me they were taking my little Bo to the NICU.
Gratefully, we had a “short stay”. His breathing resolved. He weaned off oxygen. His sugars stabilized. And, he was able to come home with us.
But, one thing I learned is that even if it’s a “short stay”…seeing your baby hooked up to life-saving equipment of any kind is imprinted on your heart and mind forever.
Before my son was in the NICU, I’d spent 6+ years around medically fragile babies and families as a NICU occupational therapist.
I want to share 6 things I realized after being there as a mom.
1. Being alone without my baby after delivery is a feeling I’ll never forget.
Of all the experiences surrounding birth, this is the feeling I remember most vividly. Laying in the delivery bed while my OB delivered the placenta and stitched me up without my baby was horrible. Honestly, I don’t have better or more eloquent words to use. I wouldn’t wish it on anyone.
For me, the experience of “recovering” immediately after birth without my baby was worse than visiting him in the NICU the first time and seeing him connected to lines and tubes.
It is unnatural. Moms should be with their babies.
Before experiencing this myself, I had never thought about it. Considering I work with moms who experience this daily, it may be shocking to hear that. But again, when it’s your work environment…we can distance ourselves from the realities.
As I look back, I’m haunted a bit by the way the delivery room felt after Bo was wheeled away. I remember my husband praying over us and our new baby, and the amazing OB and delivery team who consoled and comforted me while I cried. Labor and delivery nurses are angels.

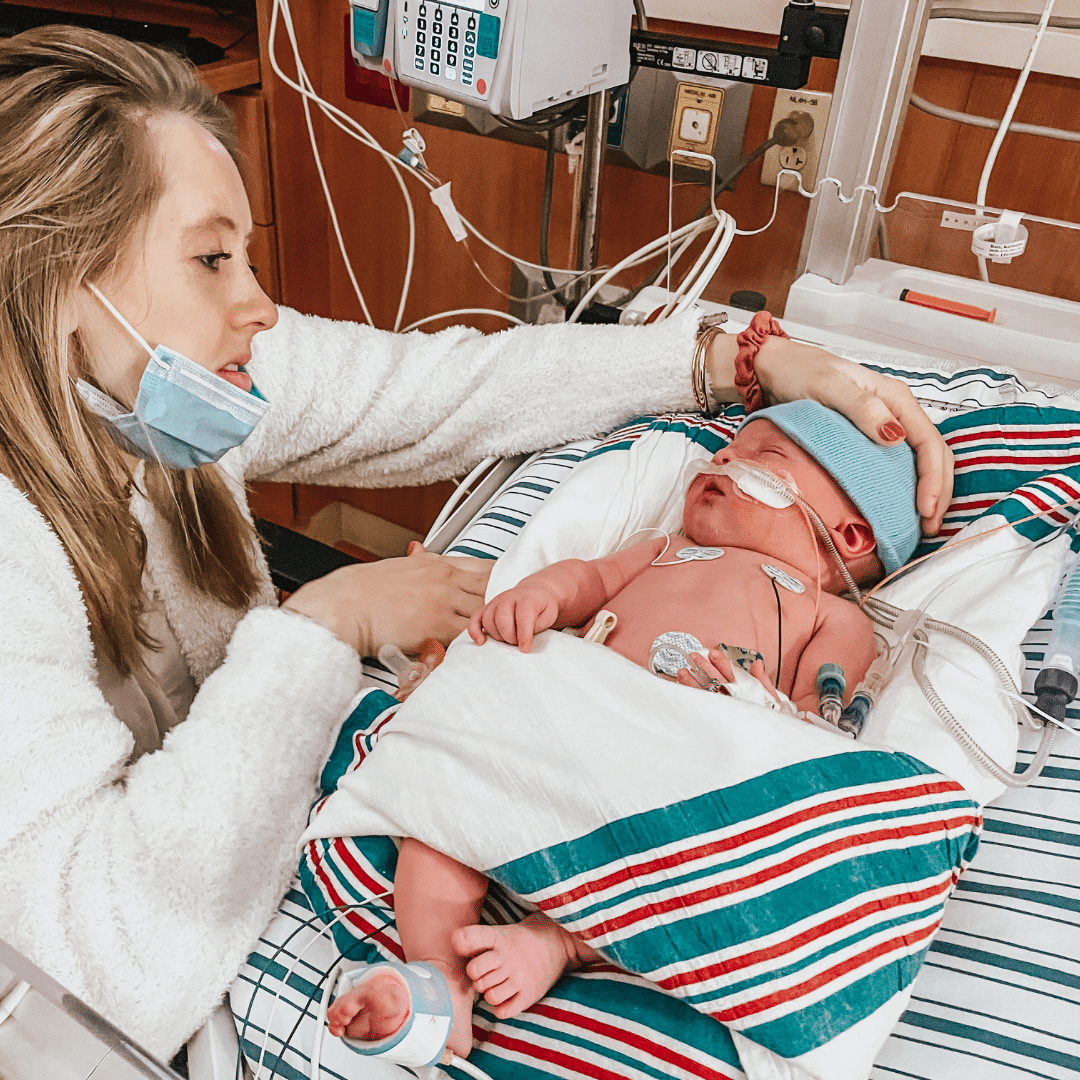
2. I don’t like looking at photos of my baby from that time.
It was months before I could look at a photo of Bo during his NICU stay without spiraling into an anxious pit. Not only did it stir up anxiety, but it didn’t even feel real. Looking back on those images, he doesn’t feel like mine.
I would see myself in a photo standing next to him, holding him…and I remember the disconnect I felt. You never know how you’re going to react in a moment until you’re there.
I don’t enjoy looking at photos from his NICU stay. It reminds me how vulnerable he was. I thought it would remind me of his resilience and the incredible strength he had as he overcame a tough delivery. Even though those things are true, seeing images of him stirs more fear than gratitude. Maybe with more time, those feelings will change. I still have healing to walk through.
If you find yourself feeling the same way about your baby, just let yourself feel it. Everyone feels and processes the NICU experience in their own way. If you’re in the NICU, reach out to the unit social worker to get connected with a counselor who can help you process the experience.


3. I felt guilty for not being at his bedside 24/7, but I also didn’t want to be.
THE GUILT! You guys, I didn’t feel guilty about him being in the NICU. I knew in my heart that was not my fault.
But, I felt guilty for not being at his bedside 24/7.
And to take it a step further, I didn’t want to be.
Whew, I type that 5 months later and still think to myself, “How could you be okay with not being at your baby’s bedside when they were JUST born and sick?”. But, it’s how I felt. And maybe there’s someone out there who is feeling the same way.
I think that question is asked by A LOT of people who have never had a sick child in the hospital.
It’s hard to be there. It’s hard to sit there all day, heal from delivery, learn to pump, interact during a vulnerable time with so many doctors and medical team members, and bond and build a relationship with your baby.
It does not make you selfish to need to step away. (Read that again!)
If you need to go home to rest or sleep in your own bed, do it!
If you want to stay on the postpartum unit and pump instead of going to the unit for a feeding session, that’s okay!
If you need to “sleep in” so you can mentally and physically prepare to be in the NICU all day, you should!
It’s not normal to live in the NICU. Take time for yourself.

4. I really cared about certain things, but not others.
If you are a NICU parent, did you find yourself really caring and getting upset by some things and not others? I did!
For example, they waited to put clothes on Bo until I was there, so I wouldn’t miss out. It was such a sweet thought that put my needs as his mom first. In reality, I didn’t really care about his first outfit.
But, when I found out he got his first bath without me, I was upset. For me, that first bath felt super important to me, but that first outfit? Not so much.
We may surprise ourselves with how we respond as parents in the NICU. Certain things may be triggering while others aren’t.
Make sure if you have preferences (like being present for the first bottle, or wanting to breastfeed), that you make them known to your baby’s team. Your baby’s nurse can’t honor what they don’t know.
5. I was worried about what the NICU staff thought of me as a mom.
Of all the realizations I had after becoming a NICU mom, this statement surprised me the most.
I was ODDLY concerned about what the NICU staff thought of me as a mom. The worry of being “judged” by the medical staff was something that came out of left field.
Especially because the staff caring for me and my baby knew me on a personal level prior to our NICU stay.
I interacted with them on a daily basis as the unit occupational therapist, and they knew how much I loved and cared for my family.
Here’s something I realized. Maybe you do too? When you’re a NICU parent, it feels like you’re in a fishbowl (does that make sense?).
As a parent, you’re sitting there perhaps in your private room, glass doors, and the medical team or nursing station is watching and walking by constantly. If you get up to look at your baby, change their diaper, or peek at their feeding…everyone knows.
I’ll be honest, I brought those feelings upon myself. No one treated me unkindly, or said anything that should stir up feelings of unworthiness. The overall experience stirred those feelings of self consciousness in my heart.
Here’s an example.
I was leaving the unit around 7:30 p.m. after spending the day there. As I was leaving with my husband, his nurse said, “Will you be back for his 11:00 feeding tonight?”.
I said, “No, we’ll be back tomorrow morning.”
I’d say that’s a typical exchange in the NICU between parents and providers, but gosh, it wrecked me. At the time, I was still on the postpartum unit one floor away from the NICU. Technically, I could have “easily” walked down later that evening for Bo’s feeding.
But at the moment, it didn’t feel easy. I wanted to be alone in my postpartum room, enjoy dinner, pump, and try to sleep.
Guilt. I was SO worried that the nurse thought I was a bad mom. And it wasn’t her fault for making me feel like that. She was kind and considerate. She simply wanted to plan her shift. She needed to know if I would be there so she could know how to prepare Bo’s feedings.
I learned that even well-intentioned words by NICU providers can stir emotions and feelings in parents that may impact their confidence, participation, and visitation.

6. I feel guilty for even saying I’m a NICU mom, knowing others have had a much longer journey.
I’ve seen a lot of babies get discharged from the NICU, and almost every single one had a longer NICU stay than mine.
I’ve witnessed the heartache and struggle of families navigating both life at home and visiting their baby. Families did it a lot longer than me.
It doesn’t feel right saying I’m a NICU mom when I’ve seen worse.
When I’ve seen families celebrate 100 days.
When I’ve celebrated first birthdays with babies on the unit.
I am grateful for the NICU parents and organizations like Dear NICU Mama and Penelope Project that validate the experiences of “short-term” NICU parents.
When I returned to work after my maternity leave three months later, I entered the NICU not only as an occupational therapist, but also as a mom who had experienced an array of emotions surrounding birth and her most precious gift in need of medical care.
My recent birth experience has brought on “a new approach” to educating as I continue working as a NICU occupational therapist and create education within the Blooming Littles’ community.
I hope hearing about my experiences as a NICU provider turned NICU mom has shed some light, hope, or perspective on the NICU experience.
You’re never alone. You’re doing an amazing job. I’m so glad you are here.