Many babies that spend time in a Neonatal Intensive Care Unit (NICU) will require additional feeding support after they discharge home.
Sometimes this comes in the form of ongoing speech therapy or occupational therapy to maintain or meet targeted feeding development goals. Other times, in addition to this, babies will need a long-term feeding tube to allow families to continue to give them the nutrition they need when they are unable or it’s unsafe to do so by mouth.
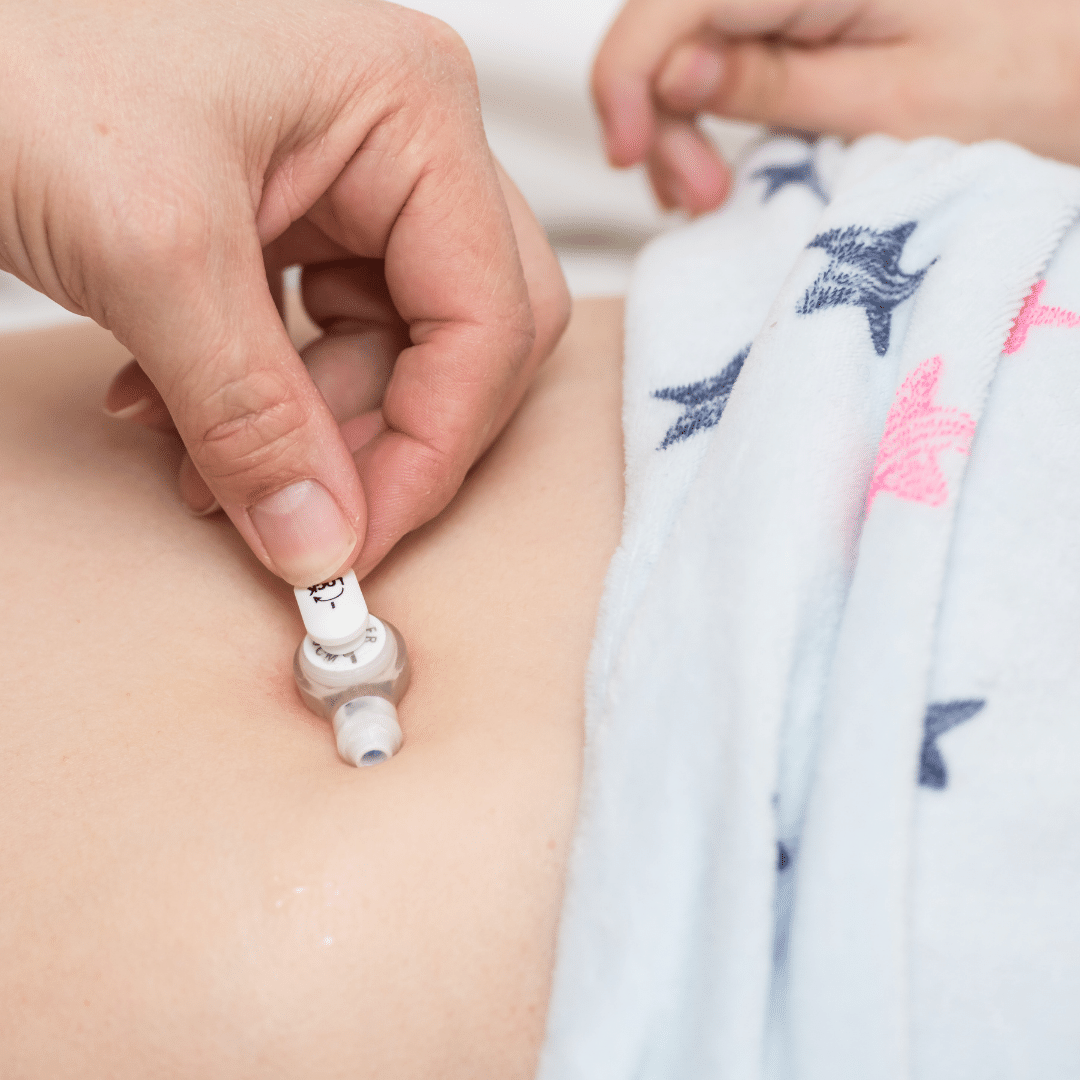
A gastrostomy tube (or G-tube) or Percutaneous Endoscopic Gastrostomy tube (PEG) are surgically placed ports in a baby’s stomach that allow families to connect a pump to their baby to continue to deliver nutrition at home. Much like a nasogastric tube (NG tube, through the nose) or orogastric tube (OG tube through the mouth) that baby had in the NICU, placement of a G-tube is safer and more developmentally appropriate for home. Families usually visit a GI doctor every few months after discharge to check on the tube and manage tube feeding recommendations.
Depending on the child’s medical state and swallow safety at discharge, they may also be able to practice bottles or breastfeeding in addition to their tube feeding regimen.
When I first started my career in a children’s hospital, the term G-tube felt something like a curse word. It’d seemed as if everyone would mouth it, whisper it, or simply gestured whenever it came up in conversation. Quite similar to “He who must not be named” in the beloved Harry Potter series. Nurses, medical teams, and families would do anything they could to get babies out of the door without a tube, even if the child wasn’t feeding well.
You may also be interested in:
HOW CAN I HELP WITH FEEDING DEVELOPMENT BEFORE MY BABY CAN SAFELY EAT?
As I transitioned into pediatric acute care, I too thought of a G-tube as a last resort, a failure, a game over. I distinctly remember feeling like I failed the patient and their family if the patient ended up needing a G-tube. I recall scouring the internet, old text books, special interest groups and colleagues trying to find where I went wrong and what I should have done differently to help my patient.
Time passed and my clinical skills strengthened. As the years went by and I began seeing my former NICU babies in our developmental follow up clinic, I started to notice a couple of trends.
Trends of families who opted in to G-tube placement:
The families who had opted for G-tube placement before discharge seemed more adjusted. The babies had healthy weights and were plotting nicely on the growth curve. Their developmental milestones were at or close to their adjusted age. And, most importantly, parents didn’t report that they despised feeding time. Many of these babies had improvements in their feeding skills and oral acceptance since discharge. And in time, many of the tubes were able to be removed.
Trends of families who chose NOT to opt in to G-tube placement:
Alternatively, the families who did not opt for tube placement continued to seem stressed and exhausted in our follow up encounters. They admitted that feeding time was not enjoyable and family members often argued over who was going to do that feeding. These babies often required supplemental oxygen for longer periods following discharge. They frequently struggled to gain weight and often began to trend down on the growth chart. Without adequate nutrition, they didn’t have the fuel to work on motor and cognitive development. Their brains weren’t getting all the nutrition they needed for optimal growth during that critical time. They often showed us signs of aversion or more concerning were sometimes readmitted with concerns for aspiration and respiratory distress.
I quickly learned that G-tubes weren’t all bad. They were actually developmentally supportive tools to help bridge the gap from hospital to home.
They were, in fact, a feeding intervention much like all of the strategies we were using at the bedside. The realization released years of guilt and helped me become a better patient advocate and family support.
Now I am able to confidently share this information with families and ease their fears regarding G-tube placement. My favorite highlights to share are that G-tubes can:
- allow feedings to stay cue based and promotes high quality feedings
- help make sure that baby gets all of the nutrition and hydration they need for brain development (which is even more important for babies born premature!)
- allow baby to conserve energy for important tasks like growing, gaining weight, and reaching developmental milestones
- decrease negative stimulation around the face and mouth (i.e. NG tube and tape)
- offer an easy back-up plan to help baby get nutrition, hydration, and medication in the event they become sick or are refusing oral intake.
- ensure that all essential medications make their way into the stomach and then into the bloodstream rather than potentially gagged and vomited out, coughed out, or spit out if they are administered by mouth.
If you and your family are finding yourselves faced with this conversation or decision, please know that you are not alone, and I know that this choice does not come easily.
you will make the decision that is right for your baby and family. I hope that my experiences and insight have helped shine a more positive light on a presumed villain with a somewhat unfair bad rap.
If you’d like to reach out for further conversation or have unanswered questions, I’d love to hear from you!